If you are reading this, chances are you or someone close to you is dealing with a stubborn cough, heavy breathing, or that uncomfortable tight feeling in the chest that just refuses to leave.
You may be searching late at night, wondering whether this is serious, whether you need medicine, or how long recovery will take. Clear answers matter right now. Patients often receive mixed advice from friends, the internet, and even old prescriptions at home.
That confusion delays the right care.
This guide brings together essential bronchitis facts in plain language, shaped around real patient concerns. You will understand warning signs, timelines, and practical bronchitis symptoms and treatment options that doctors actually recommend.
Read this as a working roadmap so you can make informed, calm decisions about your health and breathing.
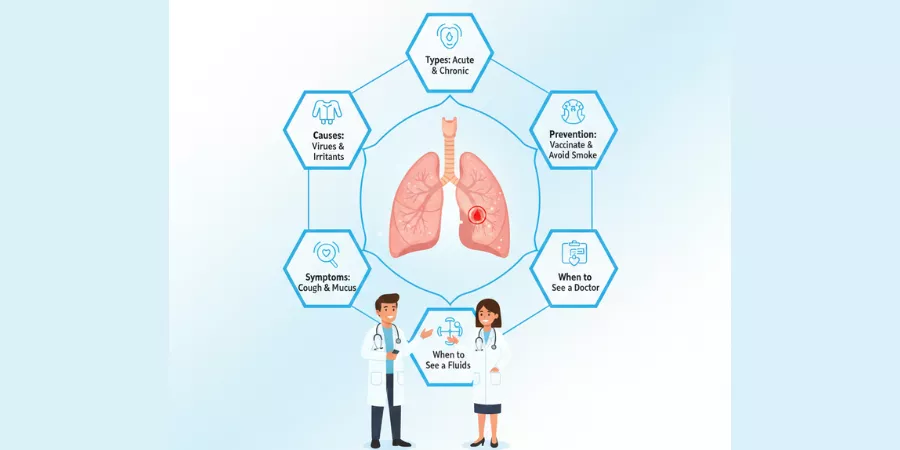
What is Bronchitis?
Bronchitis is inflammation of the airways that carry air into the lungs. In simple terms the bronchial tubes become swollen and irritated. When doctors describe this they often say the condition involves inflamed bronchial tubes that produce more mucus than usual. That extra mucus leads to a persistent cough with mucus and the heavy feeling many people call chest congestion.
Patients ask which of these are essential bronchitis facts. First, bronchitis is not always the same. Some cases are short lived and follow a cold. Other cases are long lasting and linked to smoking or repeated exposures. Recognizing which pattern fits you changes the plan. That matters because bronchitis symptoms and treatment vary by type.
Common Symptoms to Watch For
Typical signs are easy to recognize. A sudden cough often starts after a viral infection. The cough may be dry at first and then produce sputum. Other symptoms include mild fever, fatigue, and a feeling of tightness in the chest. For many people the most troubling features are the persistent cough with mucus and the chest congestion that reduces sleep quality.
Doctors list these core bronchitis facts about symptoms:
- A cough that lasts beyond a typical cold is common.
- Sputum color may change, but color alone does not prove a bacterial infection.
- Wheeze and shortness of breath suggest airway narrowing.
- Fever above 101°F or rapid worsening means seek care.
These points shape how clinicians decide if further testing or antibiotics are needed.
Causes: Viral, Bacterial, and Environmental
Most bronchitis is viral. The same viruses that cause colds and flu often travel down into the airways. That is one of the most important bronchitis facts: antibiotics do not help viral bronchitis. Antibiotic overuse leads to resistance and side effects without benefit.
Bacterial bronchitis is less common but can occur. Smoking and pollution increase risk. Repeated exposure to airborne irritants damages the lining of the bronchi and makes episodes more frequent. In people with existing lung disease bronchitis can trigger more serious problems.
Acute vs Chronic Bronchitis
Understanding acute vs chronic bronchitis is critical. Acute bronchitis usually lasts for a few days to a few weeks and often follows a cold or flu. Chronic bronchitis refers to cough with mucus for at least three months in two consecutive years and usually links to smoking or long term lung irritation.
Acute bronchitis typically resolves with supportive care. Chronic bronchitis requires a different focus. Management targets symptoms, reduces flares, and addresses underlying causes such as smoking cessation. Recognize which side of the acute vs chronic bronchitis divide you are on. That is a central piece of bronchitis facts clinicians emphasize.
How Long Does Bronchitis Last
A common question is how long does bronchitis last. For acute cases expect two to three weeks for symptoms to improve, though cough can linger for up to six weeks in some people. Chronic bronchitis follows a different timeline. Symptoms wax and wane over months or years, and flares require prompt attention.
When measuring duration doctors think in phases. Viral inflammation peaks early and slowly resolves. If symptoms worsen after a period of improvement or last far beyond expected windows, it raises concern for complications or a different diagnosis. Ask your clinician about your expected course so you know whether your recovery fits the typical pattern.
Diagnosis: What Your Doctor Will Check
Clinicians start with history and physical exam. They will ask how long the cough has lasted, whether you produce mucus, and if you have risk factors like smoking. On exam they will listen to your lungs for wheezes or crackles.
If diagnosis remains unclear your doctor may order a chest x ray or sputum test. For chronic symptoms pulmonary function tests can show airway obstruction and guide treatment choices. These steps are part of standard bronchitis facts that help avoid missed diagnoses like pneumonia or asthma.
Bronchitis Symptoms and Treatment
Treatment differs by cause and severity. For viral bronchitis antibiotic therapy is not recommended. Instead doctors advise:
- Rest and fluids to help loosen mucus.
- Humidified air or steam inhalation to relieve chest congestion.
- Over the counter pain relievers for discomfort.
- Cough medicines selectively; suppressants at night can aid sleep but should not be overused.
If bacterial infection is suspected antibiotics may be appropriate. In cases of wheeze or airway obstruction doctors may prescribe inhalers or short courses of steroids. For chronic bronchitis long term strategies include bronchodilators, pulmonary rehabilitation, and vaccinations to prevent flare triggers.
These are practical bronchitis facts to guide you through decisions. Discuss options with your clinician rather than self prescribing.
Home Care and Bronchitis Prevention Tips
Prevention is often simpler than treatment. Here are useful bronchitis prevention tips doctors recommend:
- Stop smoking and avoid secondhand smoke. Smoking remains the strongest modifiable risk factor for chronic bronchitis.
- Get annual influenza vaccination and follow guidelines for pneumococcal vaccines when appropriate.
- Wash hands frequently and avoid close contact with people who have respiratory infections.
- Use masks in high risk environments and improve indoor ventilation where possible.
- Manage chronic illnesses such as diabetes and heart disease because they increase vulnerability.
These prevention measures reduce the chance of initial illness and lower the risk of repeated episodes.
When to Seek Care
One exact long tail question is when to see a doctor for bronchitis. Seek prompt medical attention if you experience:
- High fever that does not improve.
- Shortness of breath at rest.
- Chest pain with breathing.
- Severe or worsening cough, especially with bloody sputum.
- Symptoms lasting beyond expected recovery windows.
If you have chronic lung disease or are immunocompromised consult early. Early care changes outcomes for high risk patients.
Special Considerations for Children and Older Adults
Children may dehydrate quickly when cough and fever are present. Older adults have higher risks of complications.
For both groups clinicians often take a lower threshold for evaluation. Vaccination and limiting exposure are especially important in these populations.
Myths and Clear Answers
Myth: Color of sputum proves bacterial infection. Fact: Sputum color alone is an unreliable indicator.
Myth: Cough must be suppressed at all costs. Fact: Cough clears mucus. Occasional suppression to sleep is reasonable, but complete suppression can hinder clearance.
Myth: A single episode means permanent damage. Fact: Many people recover fully from acute bronchitis; chronic changes typically require long term exposures or underlying disease.
Quick Action Plan
If you develop a new cough:
- Note onset date and associated symptoms.
- Use humidified air and fluids for comfort.
- Avoid antibiotics unless your clinician prescribes them.
- Seek care if symptoms meet the red flag list above.
These practical steps reflect core bronchitis facts clinicians want patients to know.
Frequently Asked Auestions
What causes the mucus color to change?
Immune cells and debris can alter color. This is not definitive for bacterial infection.
Are inhalers helpful?
Inhalers help if wheeze or airway narrowing is present. Your doctor will test for that.
Can bronchitis lead to pneumonia?
Yes, especially in vulnerable patients. Watch for worsening fever and breathing difficulty.
How to tell if it is chronic?
Chronic bronchitis fits the definition of cough with sputum most days for three months in two consecutive years. That guideline is a diagnostic anchor.
Conclusion
These bronchitis facts are designed to make your next clinic visit more productive. Understand whether your cough fits the acute or chronic pattern. Know the typical timeline for recovery and when to escalate care. Use the bronchitis symptoms and treatment options your doctor recommends and follow simple bronchitis prevention tips to reduce future episodes.
If you remain uncertain about symptoms or recovery, ask your clinician specifically about how long does bronchitis last in your case and whether additional testing is needed. Clear information and timely care make the difference between a brief illness and ongoing respiratory problems.