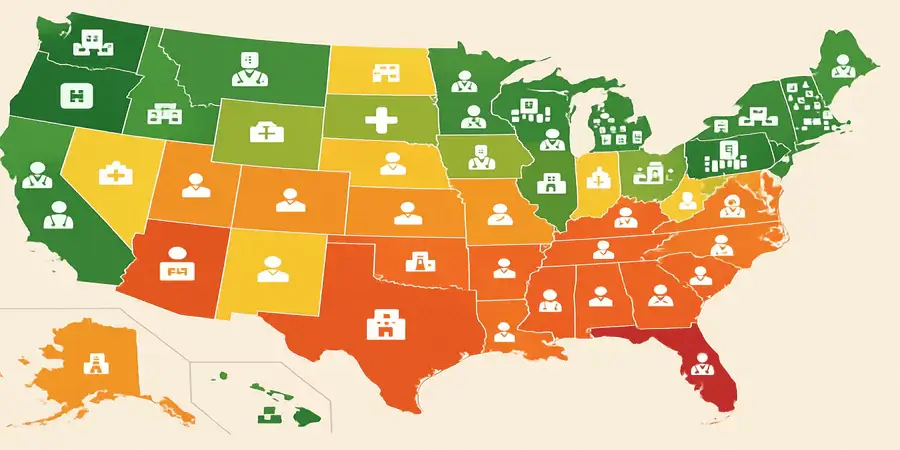
Healthcare quality and accessibility vary dramatically across the United States, with some states leading the nation in comprehensive care delivery while others struggle with significant systemic challenges. Recent comprehensive analyses reveal a stark geographic divide in healthcare performance, with profound implications for millions of Americans seeking quality medical care.
Top-Performing States: Excellence in Healthcare Delivery
What state has the best medical care?
The National Leaders
New Hampshire┬Āhas emerged as the nation’s top healthcare state, earning this distinction through remarkable achievements in affordability and access. The state boasts the lowest average monthly health insurance premium at approximately $470 and ranks fourth nationally for the lowest out-of-pocket medical expenses. New Hampshire demonstrates exceptional provider availability with the fifth-highest nurses per capita and sixth-highest physician assistants per capita.
Massachusetts┬Ācontinues its legacy of healthcare excellence, topping the Commonwealth Fund’s 2025 scorecard and maintaining its reputation for universal health coverage initiatives. The state excels across multiple healthcare dimensions and serves as a model for comprehensive care delivery.
Rhode Island┬Āsecures second place nationally, with residents allocating only 5.6% of their income to out-of-pocket medical costsŌĆöthe lowest rate in the country. The state features high insurance rates for both adults and children, along with the sixth-highest ratio of physicians per capita and substantial numbers of geriatricians.
Key Performance Indicators of Leading States
The best-performing states share several critical characteristics:
- Comprehensive Insurance Coverage:Low uninsured rates and affordable premium options
- Strong Provider Networks:High ratios of healthcare professionals per capita
- Preventive Care Excellence:Superior vaccination rates and screening programs
- Health Outcomes:Lower rates of chronic diseases and better life expectancy
- Accessibility:Abundant urgent care facilities and convenient care clinics
Worst-Performing States: Systemic Healthcare Challenges
The Bottom Tier
Mississippi┬Āconsistently ranks at the bottom of national healthcare assessments, facing multiple interconnected challenges. The state struggles with one of the highest uninsured rates in the nation, limited access to healthcare facilities, and chronic public health issues including elevated rates of diabetes and obesity.
West Virginia┬Āpresents a particularly troubling case, ranking as the worst state for healthcare overall despite ranking second for accessibility. The state suffers from the highest mortality rate nationally at 1,116 deaths per 100,000 residents and the worst diabetes mortality rates. Additionally, West Virginia has the fourth-highest average private health insurance premiums at $10,563 annually.
Alabama, Texas, and Alaska┬Ācomplete the bottom five, each facing distinct challenges ranging from limited rural healthcare infrastructure to workforce shortages and geographic barriers to care.
Common Challenges in Low-Performing States
The worst-performing states exhibit several concerning patterns:
- High Uninsured Rates: Significant populations without healthcare coverage
- Provider Shortages:Insufficient numbers of healthcare professionals, especially in rural areas
- Geographic Barriers:Long travel distances to access specialized care
- Economic Constraints:Higher poverty rates limiting healthcare affordability
- Chronic Disease Burden:Elevated rates of preventable conditions
Regional Healthcare Disparities
Geographic Healthcare Divide
The data reveals a pronounced regional pattern in healthcare performance.┬ĀEight of the ten worst-performing states cluster in the South and Southeast, while top-performing states are distributed more evenly across the Northeast, Midwest, and West. This geographic concentration suggests systemic regional factors affecting healthcare delivery.
Rural vs. Urban Healthcare Access
Rural communities face disproportionate healthcare challenges compared to urban areas. As of September 2024,┬Ā66.33% of Primary Care Health Professional Shortage Areas were located in rural areas. Rural residents must often travel significant distancesŌĆösometimes up to 100 kilometersŌĆöto access specialized healthcare services.
Key rural healthcare challenges include:
- Transportation Barriers:Limited public transit and long travel distances
- Workforce Shortages:Severe shortages of healthcare professionals
- Infrastructure Limitations:Poor broadband connectivity affecting telemedicine access
- Economic Constraints:Higher poverty rates and limited insurance options
The Impact of Medicaid Expansion
Coverage Gains and Economic Benefits
Medicaid expansion has proven crucial for healthcare access improvement. Forty-one states and Washington D.C. have expanded Medicaid eligibility under the Affordable Care Act, resulting in significant coverage gains. States that expanded Medicaid have not experienced significant increases in state spending while seeing tax revenue increases and overall healthcare spending declines.
The expansion has generated substantial economic benefits:
- Multiplier Effect:Every Medicaid dollar spent generates over a dollar’s worth of economic activity
- Employment Growth:Drives job creation in the healthcare sector
- Reduced Uncompensated Care: Hospitals in expansion states had uncompensated care costs of 2.7% versus 7.3% in non-expansion states
- Tax Revenue Generation:Creates additional state and local tax revenue
Non-Expansion State Consequences
The ten states that have not adopted Medicaid expansion continue to face significant challenges. These states leave substantial federal funding on the table while their residents experience higher uninsured rates and reduced access to care, particularly affecting low-income working adults who fall into the “coverage gap.”
Health Equity and Disparities
Racial and Ethnic Healthcare Disparities
Healthcare disparities persist across racial and ethnic lines in all states.┬ĀIn 42 states and D.C., avoidable mortality for Black people is at least twice the rate for the group with the lowest rate. The Commonwealth Fund’s analysis reveals that:
- Hispanic people had worse access to care than non-Hispanic White people for 79% of access measures
- American Indian and Alaska Native people had worse access for 50% of measures
- Black people had worse access for 53% of measures
Income-Based Disparities
Economic factors significantly impact healthcare access:
- People with only public insurance had worse access than those with private insurance for 44% of measures
- People without insurance had worse access than those with private insurance for 71% of measures
- Females generally had better access to care than males for 43% of measures
Future Threats and Challenges
Policy Threats to Progress
Despite historic gains in insurance coverage, healthcare experts warn of significant threats ahead. Proposed federal policy changes could jeopardize recent progress, including:
- Medicaid Funding Cuts:Proposed $880 billion in cuts over ten years could reduce GDP by $95 billion
- Work Requirements:Additional bureaucratic barriers to coverage
- Marketplace Reductions:Decreased support for health insurance marketplaces
- Premium Subsidy Expiration:End of pandemic-era affordability enhancements
Emerging Health Challenges
New challenges continue to emerge:
- Childhood Vaccination Decline:Most states experienced drops in childhood vaccination rates between 2019 and 2023
- Infant Mortality Increases:Twenty states saw worsening infant mortality rates between 2018 and 2022
- Workforce Shortages:Ongoing shortages of healthcare professionals, particularly in rural areas
Conclusion
The state of American healthcare reveals a nation of stark contrasts, where geography significantly determines health outcomes and access to care. While leading states like New Hampshire, Massachusetts, and Rhode Island demonstrate that excellence in healthcare delivery is achievable through comprehensive policy approaches and adequate funding, the persistent challenges in states like Mississippi, West Virginia, and Alabama highlight the urgent need for targeted interventions.
The success stories of Medicaid expansion states and the comprehensive approach taken by top-performing states provide clear roadmaps for improvement. However, the threats posed by potential federal funding cuts and the persistent rural-urban divide require immediate attention from policymakers at all levels.┬ĀWhere Americans live should not determine their access to quality healthcare, yet current data reveals this remains a fundamental challenge requiring coordinated federal and state action to ensure equitable health outcomes across all communities.